
According to a 2007 UFSBD study, nearly 1 in 2 French people suffer from gum problems.
In addition to local inconvenience, these periodontal diseases are important risk factors for other very serious pathologies.
It is essential to detect, diagnose and treat these conditions.
FIRST OF ALL, WHAT IS PERIODONTITIS?
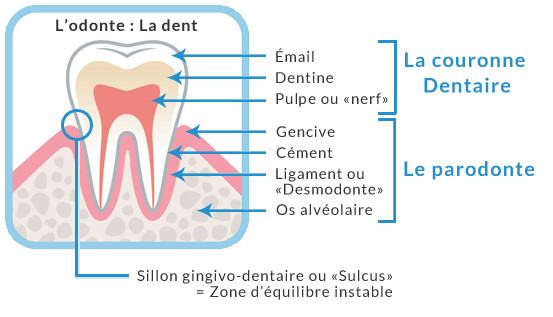
These are simply the supporting tissues of the teeth: the gum, the ligament (which connects the tooth to the gum and the bone), the alveolar bone, and the cementum (thin layer of hard tissue along the root).
The human periodontium is the site of an unstable balance between the host's (the patient's) defences and the microbial mass (bacteria and micro-organisms).
This balance can easily be upset, either by an alteration of the defences or by a quantitative or qualitative change in this microbial mass.
WHAT HAPPENS WHEN THIS BALANCE IS UPSET?
The first stage of periodontal disease is marked by inflammation of the gums, which become swollen, red and smooth (whereas normally they are pale pink and pitted). The most obvious sign of gum inflammation is that the gums start to bleed easily. Either when brushing (if it is effective), or when a little stimulation is given (with an interdental stick for example). This is GINGIVITY.
The most common cause of gingivitis is poor hygiene and the accumulation of plaque.
Repeated bleeding from the gums is ANMAL, and if it persists, you should seek medical attention.
Indeed, it is an easily treatable pathology, and if caught in time, it will not leave any sequelae.

This gingivitis affects 1 out of 2 French people and in 1 out of 2 cases, this gingivitis ends up getting worse.
GINGIVITIS WILL DEVELOP INTO PERIODONTITIS
Under the pressure of the inflammation, the system that attaches the gum to the tooth and the bone will break down, and a pocket will form, which is called a periodontal pocket. This pocket can become very deep (up to 8-9 mm) and within this pocket, bacteria will be able to develop and benefit from a favourable ecosystem. In the absence of oxygen, anaerobic bacteria will become dominant. These bacteria will organise themselves and colonise the surface of the root, which will then form subgingival tartar (which is black).
The inflammation that results from this bacterial growth is so great that the bone that supports the teeth will shrink, as if it were fleeing from this microbial attack. It is our own cells (osteoclasts) that turn against the bone and destroy it. Periodontitis is almost an auto-immune disease.
This bone loss occurs insidiously, usually without pain, sometimes with a periodontal abscess that may resolve spontaneously. It is a chronic disease, which can last for years.

Unfortunately, this bone loss is IRREVERSIBLE, and without treatment it can lead to the spontaneous loss of all teeth. This is commonly known as tooth loosening.
Bad breath is very common in periodontitis.
It is estimated that 25% of French people suffer from periodontitis.
WHAT ARE THE CONSEQUENCES FOR GENERAL HEALTH?
Although little known to the French, periodontal disease is a serious and frequent pathology that can have serious consequences. They are responsible for almost 40% of dental extractions and can cause serious complications for the patient's general health.
In fact, bacterial debris present in the periodontal pocket (lipopolysaccharides) will pass into the bloodstream and lead to chronic inflammation which favours the appearance of other more general diseases.
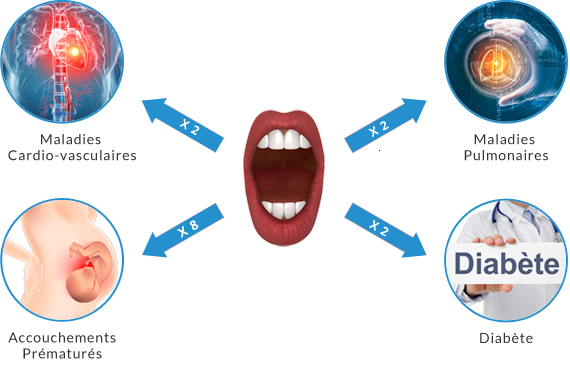
4 links have been formally demonstrated to date(source):
- a patient suffering from periodontitis has twice the risk of developing type 2 diabetes (conversely, a diabetic patient has 4 times the risk of developing periodontitis). Nearly 4 million French people have type 2 diabetes.
- a patient with periodontitis is 8 times more likely to give birth prematurely, or to have a low birth weight baby. Inflammatory diseases (of which periodontitis is one) are thought to be responsible for 40% of premature deliveries.
- a patient suffering from periodontitis has twice the risk of suffering from a chronic respiratory disease (COPD: Chronic Obstructive Pulmonary Disease, fifth cause of death in the world).
- a patient with periodontitis has twice the risk of having a stroke or a heart attack. When one has periodontitis, the risk of dying of a cardiovascular disease within 10 years is multiplied by 4.
According to a study by DeStefano on 20749 subjects in 1993, the risk of overall mortality was increased by 50% in a mixed American population (25-74 years) with periodontitis. Mortality increases by 50% for every 20% increase in average bone loss.
Links are still being investigated, but there are strong indications that periodontitis plays a role in the development of rheumatoid arthritis, certain cancers, and even Alzheimer's disease.
In 2013, the University of Lancashire in the UK published an incredible study. They studied the brains of 20 patients within 12 hours of their deaths. There were 10 patients with Alzheimer's disease, and 10 patients without. To their amazement, they found in 4 of the brains of the Alzheimer's patients, breakdown lipopolysaccharides from Porphyromonas gingivalis. One of the main bacteria involved in periodontitis.
It is therefore a real public health problem.
WHAT CAUSES PERIODONTITIS?
It is a multifactorial disease, and we still don't know exactly how and why gingivitis will develop into periodontitis, but what we must remember is that without micro-organisms, there would be no disease.
Nevertheless, several factors have been clearly identified:
- poor oral hygiene (main factor in gingivitis)
- smoking (14-fold increase in risk according to some studies)
- stress
- impaired chewing (10% more periodontitis for each missing tooth not replaced)
- hyposialia (decrease in saliva flow, beware of antidepressants and other anxiolytics which often cause this side effect). Saliva plays a very important role in the line of defence against micro-organisms.
- Diabetes (risk multiplied by 4, and it has been shown that treating periodontitis in a diabetic allows better control of blood sugar)
- obesity (and/or a diet too rich in fat)
- Gastroesophageal reflux disease (GERD: acid reflux from the stomach, which will modify the oral flora by lowering the pH)
- ENT problems can lead to mouth breathing (the nose is blocked), and thus to nocturnal hyposialia
- hypothyroidism
- Vitamin D deficiency (at least 1/3 of the French population is deficient)
- lipid imbalance(hypercholesterolemia in particular)
- all pathologies with reduced immunity (Neutropenia, AIDS, chemotherapy, etc.)
- menopause (probably related to the drop in oestrogen)
- treatment with bi-phosphonates, a treatment for osteoporosis and certain cancers (link not yet proven but strong presumptions)
- a genetic predisposing factor has been identified (allele coding for an overexpression of IL-1: PST test), but it is not very predictive (many patients carrying this gene do not develop the disease, so periodontitis is not a fatality)
This is why it is fundamental to insist on the importance of prevention in the management of this type of disease. It is essential to act before the infection occurs, as the periodontium does not regenerate.
HOW IS PERIODONTITIS TREATED?
The treatment of periodontitis is carried out in several stages.
- Prophylactic assessment: during this first consultation, the practitioner will make a precise diagnosis based on examinations involving a saliva test to measure the acidity of the saliva, its flow, its buffering capacity, and possibly a bacterial test to identify pathogenic microbes. In addition, a questionnaire is conducted with the patient to find out about their eating habits and brushing methods.
- This step will also allow the patient to become the actor of his own treatment, the control of dental plaque on a daily basis is the key to success.
- Mechanical treatment: this combines classical methods involving scaling, spraying with bicarbonate and salts and polishing the affected teeth.
- Root planing: This technique consists of intervening directly at the roots to eliminate toxins and bacterial contents via ultrasound instruments. This procedure cleans the periodontal pocket and allows the gums to re-adhere to the tooth.
- Chemical treatment: from the beginning of the treatment the patient will use pastes (based on bicarbonate and hydrogen peroxide) and antiseptics. During the surfacing in the following sessions, the gum will be irrigated, then rinsed with povidone-iodine, a powerful antiseptic. In some cases, a targeted antibiotic therapy will complete the treatment.
